Specialties: prenatal examination, delivery, pre-pregnancy examination, infertility test, artificial insemination, IVF, frozen eggs, frozen embryos, minimally invasive laparoscopic gynecological surgery, hysteroscopic surgery (including cold knife), cervical smear/HPV examination and vaccination, menstrual abnormalities, ovarian function assessment
Ovarian
endometrioma (chocolate cyst) is a health concern for many women, especially
those planning for pregnancy. It raises concerns about fertility and whether
surgery is necessary before attempting conception. Should you undergo surgery
first or consider egg freezing? Here’s a comprehensive guide to making an
informed decision.
What is Endometriosis?
Endometrial
tissue normally grows inside the uterus, shedding monthly during menstruation.
However, in endometriosis, this tissue abnormally implants outside the uterus—such
as on the ovaries, fallopian tubes, pelvis, and even other organs. These
implants respond to hormonal fluctuations, causing chronic inflammation,
adhesions, pelvic pain, infertility, and other complications.
How Does Ovarian Endometrioma Affect Fertility?
Endometriosis
affects approximately 10% of women of reproductive age, with 30-50% of patients
experiencing infertility. Studies suggest that spontaneous conception rates in
women with endometriosis may drop to as low as 1-10%. Ovarian endometrioma, a
common manifestation of endometriosis, can impact fertility in several ways:
- Reduced Ovarian Reserve: Chronic inflammation
damages normal ovarian tissue, leading to a decline in follicle count and
an increased risk of diminished ovarian reserve (DOR). Anti-Mullerian
hormone (AMH) blood tests help assess ovarian reserve—higher levels
indicate more available eggs.
- Impaired Ovulation and
Fertilization:
The inflammatory environment disrupts follicular development and
ovulation, reducing fertilization rates.
- Blocked Fallopian Tubes: Adhesions may cause tubal
obstruction, preventing sperm and egg from meeting.
- Increased Risk of
Miscarriage:
Impaired endometrial receptivity makes embryo implantation more difficult,
increasing pregnancy loss risks.
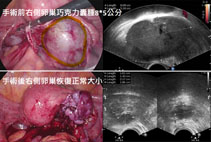
The Impact of Surgery on Ovarian Function
When
medical treatment fails, surgery is often recommended to remove ovarian
endometriomas and alleviate symptoms. While surgery can improve quality of
life, it may also compromise ovarian function, and endometriosis has a high
recurrence rate, sometimes necessitating repeat surgeries. Medication after
surgery can help reduce recurrence risks.
After
surgery, ovarian function may decline, especially if multiple surgeries are
performed. This can lead to a lower egg yield in future fertility treatments.
For young women who have not yet had children or those with already diminished
ovarian reserve, egg freezing before surgery is strongly recommended to
preserve fertility.
Egg Freezing vs. Surgery: Which Should Come First?
The
decision depends on factors such as age, ovarian function, and symptom
severity.
When
to Consider Egg Freezing First
- Age 30-35 with a
reasonable ovarian reserve, concerned about future fertility decline.
- Cysts ? 4 cm, minimal symptoms,
no immediate pregnancy plans but wish to preserve fertility.
- History of previous
ovarian surgery, concerned about further ovarian reserve depletion.
- Regular follow-ups are
necessary post-freezing to monitor cyst growth and determine surgical
needs.
When
to Consider Surgery First
- Cysts > 5 cm or rupture
detected.
- Severe pain affecting
daily life, unresponsive to medication.
- Ovulatory dysfunction due
to the cyst, causing infertility for over six months.
- Imaging suggests
malignancy risk.
- Stable follow-ups after
surgery, with medication to delay recurrence, followed by egg freezing
evaluation.
- Planning for IVF, where
cyst location might interfere with egg retrieval, necessitating prior
surgery.
Q&A: Common Concerns
Q1: Can I still conceive naturally after surgery?
A:Most women can still conceive
naturally, but ovarian reserve may decline. Assisted reproductive technologies
(ART) may be needed if fertility is compromised. Multiple surgeries further
reduce pregnancy chances, so egg freezing before surgery is advisable.
Q2: Does surgery affect IVF success rates?
A: A systematic review by Hamdan
et al. (Human Reprod Update, 2015) compared IVF outcomes in women with and
without ovarian endometrioma surgery. Results showed no significant difference
in live birth or miscarriage rates. However, women with endometriosis had fewer
retrieved eggs post-surgery. Discussing ovarian reserve status with a
reproductive specialist before surgery is crucial for planning an optimal IVF
treatment strategy.
Q3: If I freeze my eggs, will I still need surgery later?
A:Successful egg freezing
requires regular follow-ups. Surgery should be reconsidered only if cysts grow
significantly or meet surgical criteria.
Q4: Will the cyst continue to grow if I don’t opt for surgery?
A:Not necessarily. Disease
progression varies; some cysts remain stable, while others enlarge. Regular
ultrasound monitoring helps determine the need for surgery.
Conclusion: Personalized Treatment Decisions Matter Most
Every
woman’s situation is unique—factors such as age, cyst characteristics,
symptoms, and fertility goals must be considered. Consulting a reproductive
specialist to evaluate ovarian function and create a tailored fertility plan is
essential.
Key Takeaways
- Ovarian endometrioma can
reduce ovarian function and pregnancy chances.
- Egg freezing before
surgery
is advisable for women who are not yet ready for pregnancy but want to
preserve fertility.
- Surgery first is recommended for large
cysts or cases with significant health impacts, followed by a reassessment
of fertility preservation options.
- Surgery may reduce ovarian
reserve, impacting egg yield. Using anti-adhesion agents and hemostatic
techniques during surgery can help minimize damage. Post-surgical
medication can delay recurrence. A personalized treatment approach,
discussed with your doctor, is critical.
If
you’re struggling with ovarian endometrioma and fertility concerns, consult a
reproductive specialist early. Seizing the right timing can help you create the
best fertility plan for your future!